 The Department of Health and Human Services’ (HHS) Health Resources and Services Administration (HRSA) previously announced the distribution of $5 billion in Provider Relief Fund (PRF) payments to eligible skilled nursing facilities to protect residents from the impact of COVID-19.
The Department of Health and Human Services’ (HHS) Health Resources and Services Administration (HRSA) previously announced the distribution of $5 billion in Provider Relief Fund (PRF) payments to eligible skilled nursing facilities to protect residents from the impact of COVID-19.
On August 27,2020, HHS distributed the initial $2.5 billion of this funding to support facilities’ COVID-19 infection control efforts, including by conducting appropriate testing, acquiring necessary personal protective equipment (PPE), investing in staff, and establishing COVID-19 isolation facilities. Eligible facilities automatically received a per-facility payment of $10,000 plus a per-bed payment of $1,450 in this initial distribution.
On September 3, 2020, HHS announced that the next $2 billion incentive payment allocation would be based on measuring nursing home performance through required nursing home data submissions and distributing payments based on these data. Data submissions will come from the Certification and Survey Provider Enhanced Reports (CASPER), Nursing Home Compare (NHC), and Provider of Services (POS) systems. Nursing homes will not have to apply to receive a share of this incentive payment allocation. Additional details were recently added to the HHS PRF website as follows:
Eligibility for Payment
In order for a facility to be eligible for payment, they must pass two initial gateway qualification tests on both their rate of infection and rate of mortality.
- First, a facility must demonstrate a rate of COVID infections that is below the rate of infection in the county in which they are located. This benchmark requirement for infection rate reflects the goal of the incentive program to recognize and reward facilities that establish a safer environment than the community in which they are located.
- Second, facilities must also have a COVID death rate that falls below a nationally established performance threshold for mortality among nursing home residents infected with COVID.
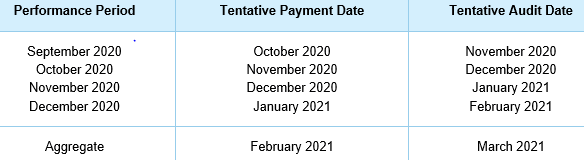
Payment Periods
Infection Measure Calculation
For facilities that meet the gateway criteria, their COVID infection performance will be measured by assessing two factors: the amount by which their own infection rate is lower than their county’s infection rate and total patient volume, as measured by resident-weeks. In a given performance period, a facility’s infection rate will be measured as their total number of COVID infections (not including COVID admissions) divided by their total count of resident-weeks reported in NHSN.
The difference between the facility’s and county’s infection rates is then scaled upward by the facility’s patient volume, as measured by resident-weeks, which yields the facility’s performance score on the infection measure.
Mortality Measure Calculation
Facilities are eligible for evaluation of their COVID mortality performance in a given performance period if they meet the gateway criteria and have at least one non-admission COVID infection. For these facilities, their mortality performance calculation will rely on two main pieces of information from NHSN data: the total number of COVID deaths resulting from in-facility infections and the total number of non-admission infections. Infected patients will be counted if they occur in an extended block of time, covering the performance period and several weeks preceding the performance period. These two pieces of information will be used to measure a preliminary COVID mortality rate for each facility. Direct outreach will be conducted to facilities that have at least one death in the performance period and have a mixture of COVID admissions and in-facility infections. The goal of this outreach will be to ascertain how many of their reported COVID deaths were due to in-facility infections versus COVID admissions.
These facility level characteristics will be incorporated with relevant health and demographic characteristics for each facility’s resident population into a statistical model that will be used to estimate the expected number of deaths for each facility in the performance period.
- Facilities with a mortality rate significantly exceeding expectations will become ineligible for any incentive program payments in the performance period.
- Facilities with lower mortality than expected will be eligible for payment, which will be scaled up based on the amount by which they fall below the expected number of deaths.
Incentive Payment Calculation
For each performance period, the total available bonus payments will be determined based on aggregate performance on the infection measure. This total will then be split into separate payment pools for performance on the infection and mortality measures.
- First, 80% of bonus payments will be available to providers that have positive performance on the infection measure. As discussed in previous sections, these payments will be made available to any facility that meets the gateway criteria.
- Second, 20% of bonus payments will be available to providers that have positive performance on the mortality measure. Providers scoring below a threshold level of performance on the mortality measure will be deemed ineligible for payment in both the infection and mortality payment pools.
Terms and Conditions
As with other PRF payments, within 90 days of receiving this payment, you must sign an attestation confirming receipt of the funds and agreeing to the Terms and Conditions of payment which are the same as the $2.5 billion distribution on August 27, 2020. Should you choose to reject the funds, you must also complete the attestation to indicate this. These quality incentive payments may only be used for the infection control expenses. These include costs associated with the following:
- Administering COVID-19 testing for both staff and residents.
- Reporting COVID-19 test results to local, state, or federal governments.
- Hiring staff to provide patient care or administrative support.
- Incurring expenses to improve infection control, including activities such as implementing infection control “mentorship” programs with subject matter experts, or changes made to physical facilities.
- Providing additional services to residents, such as technology that permits residents to connect with their families if the families are not able to visit in person.
The HHS guidance on the provider relief funds has been ever changing and often conflicting. The FAQs continue to be updated frequently. HW&Co. is here to assist you in any way we can. Please visit the HW&Co. Current Events Center on our website for additional resources or contact your HW Healthcare Advisor if you need assistance.






