[vc_row][vc_column][vc_column_text]
There are only 75 days until October 1, 2019 when the Patient Driven Payment Model (PDPM) replaces the current PPS RUG-IV Medicare payment system. There have been countless articles and a myriad of training on PDPM. With less than three months until implementation, now is a good time to step back and assess your level of preparedness. In order to help ensure you are ready, we are providing this overview of a very complex system as well as our top 5 items that should be addressed now to prepare you for success under PDPM.
PDPM represents the biggest change to Medicare in over 20 years and will cause major changes to nursing facility operations. PPS payments were based primarily on the amount of therapy provided to a patient, regardless of the patient’s unique clinical characteristics. PDPM strives to improve payment accuracy and appropriateness by focusing on the patient clinical aspects of care, rather than the volume of services provided. It is important to note that CMS will be focusing and monitoring outcomes rather than volume of services delivered.
Major differences between the two systems:
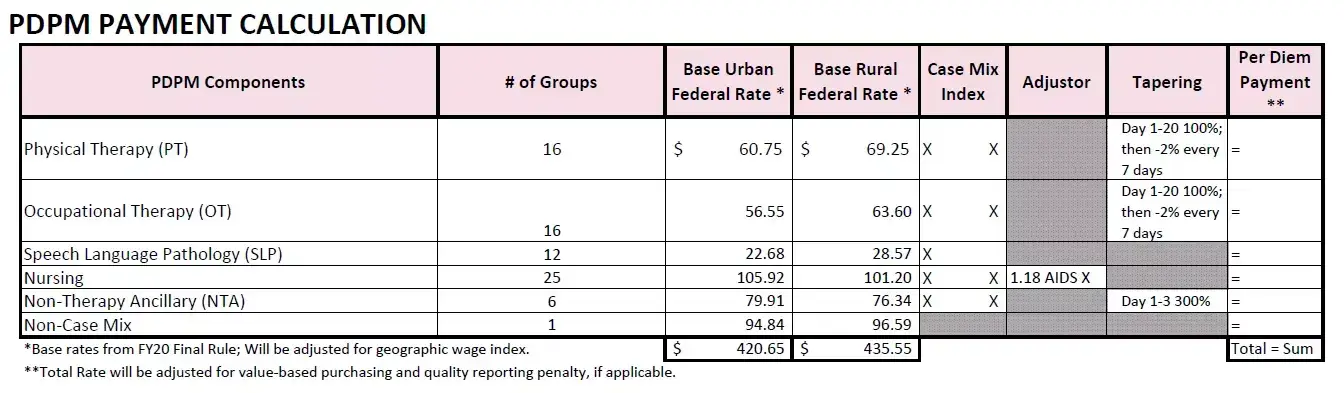
Understanding how residents group into the 6 rate components:
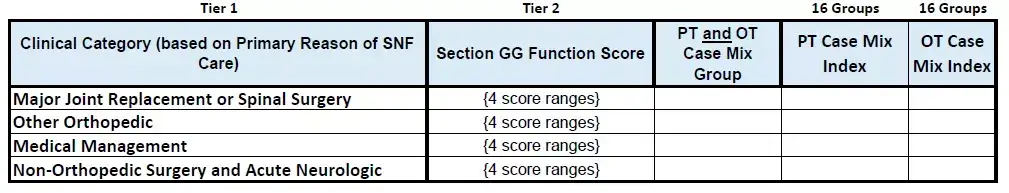
1. & 2. Physical (PT) and Occupational (OT) Therapy Components:
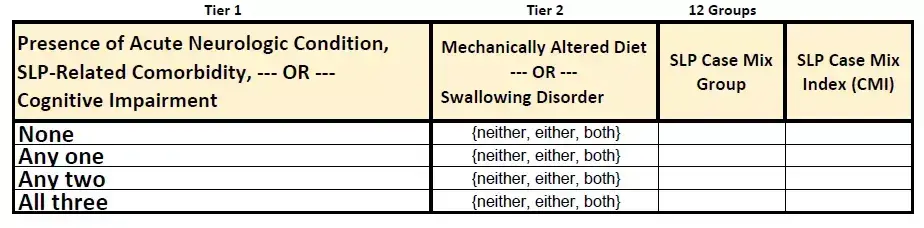
3. Speech-Language Pathology (SLP) Component:
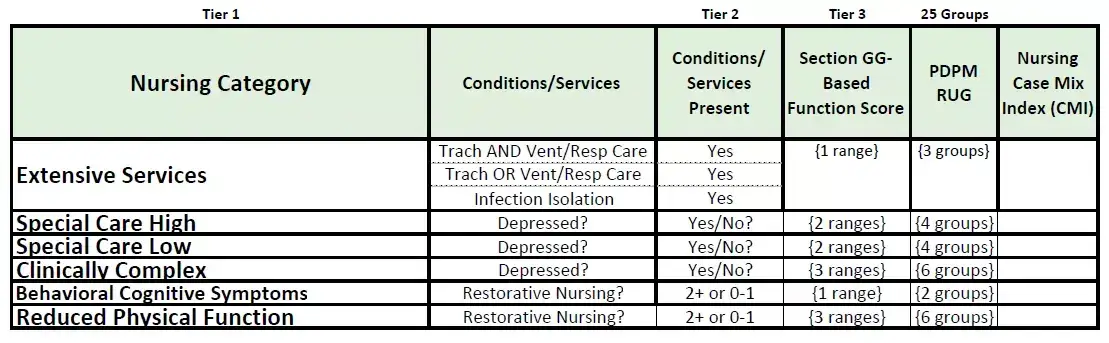
4. Nursing Component
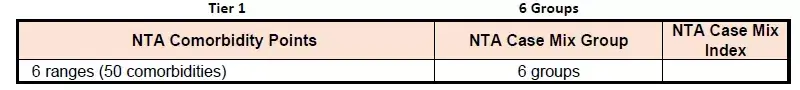
5. Non-Therapy Ancillary (NTA) Component:
6. Non-Case Mix Component: Flat rate for all residents.
PDPM payment calculation including when rate tapering kicks in:
PDPM MDS Assessment Schedule:
Click here to download PDPM At A Glance
Transition Period
There is no transition period for PDPM. October 1, 2019, is a HARD STOP. All traditional Medicare A residents skilled on October 1, 2019, will be required to have a PDPM Interim Payment Assessment (IPA). The first 3 days of October count as the beginning of PDPM stay regardless of admission data and will include 300% of the Non-therapy Ancillary rate. The Assessment Reference Date (ARD) should be set between 10/1 and 10/7, with 14 days to complete and 14 days to submit. Be aware that a RUG score is required to bill up to and including September 30, 2019. Be sure that you plan not only for this extra volume of assessments in October, but also how to best manage setting the ARD over your entire skilled census to distribute the workload.
Top 5 keys to success:
- Inter-disciplinary approach:
Capturing data timely and accurately is the most important key to success under PDPM. This cannot be done without an inter-disciplinary approach to assessing the resident particularly Section GG which was often done only by therapy. Complete and accurate assessments will require input from not only nursing and therapy but also the resident and family.
- Initial 5-day assessment:
The 5-day assessment will effect payment for the entire stay unless an optional IPA is completed. There is no longer a 14-day assessment to capture errors and omissions. You should review your procedures for getting information from the hospital (i.e. surgery data), resident and family so you can make sure you capture all key information in the 5-day assessment. You should critically review and enhance your admission and pre-admission process. A good way to identify problem areas is to compare your current 5 and 14-day assessments to determine items that were not captured timely. - Accurate ICD-10 coding:
The importance of accurately coding the primary reason for admission, as well as all clinical conditions cannot be stressed enough. Incorrect coding leads to inaccurate mapping for the PT/OT/ST components and also impacts the Nursing and NTA components. In addition, you must make sure the ICD-10 code maps to a clinical category. Otherwise, you get a “Return to Provider” code which equals no payment.Be sure you have provided adequate training to personnel responsible for ICD-10 coding. - Function codes on Section GG:
Section GG calculates function score and should reflect resident performance over 3 days, or until therapeutic intervention. It is important to adapt an inter-disciplinary approach to Section GG completion and ensure that all personnel understand the scoring. Unlike PPS, there is not a “rule of thumb” as to which category will result in a higher case mix index. This section of the MDS relies on accurate coding of several mobility and self-care items that impact the PT, OT and Nursing components. For the PT and OT components, it is better to be more independent, whereas for Nursing it is better to be more dependent. Staff education is critical here since the scoring is reversed from Section G and there are different definitions as to what constitutes an assist, etc. Bottom line is that Section GG needs to accurately represent the resident’s function level. - Capturing Co-morbidities and depression:
Under PPS, capturing co-morbidities and depression based upon mood interviews generally did not have a large impact reimbursement. Not surprisingly, facilities were not doing a good job of capturing these items since they did not translate to enhanced payment rates. Under PDPM, they can substantially increase reimbursement. Facilities should analyze and enhance their ability to conduct mood interviews and ensure they are coding all clinical conditions.
Please contact your HW Healthcare Advisor, or Paula Reape, if you would like additional information on any of the items discussed in this PDPM overview.
In addition, there will be high-level overviews of PDPM during both of the educational opportunities listed below.
Click Here to Register for Evolve, Adapt, Change
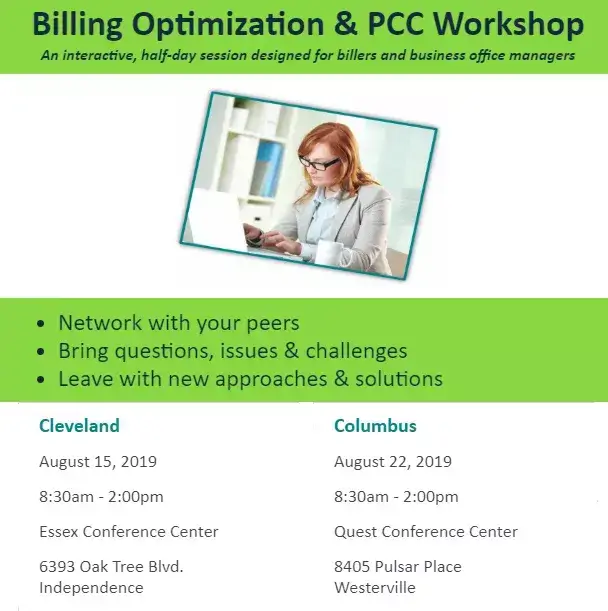 Cleveland Registration Columbus Registration
Cleveland Registration Columbus Registration

preape@hwco.com
[/vc_column_text][/vc_column][/vc_row]