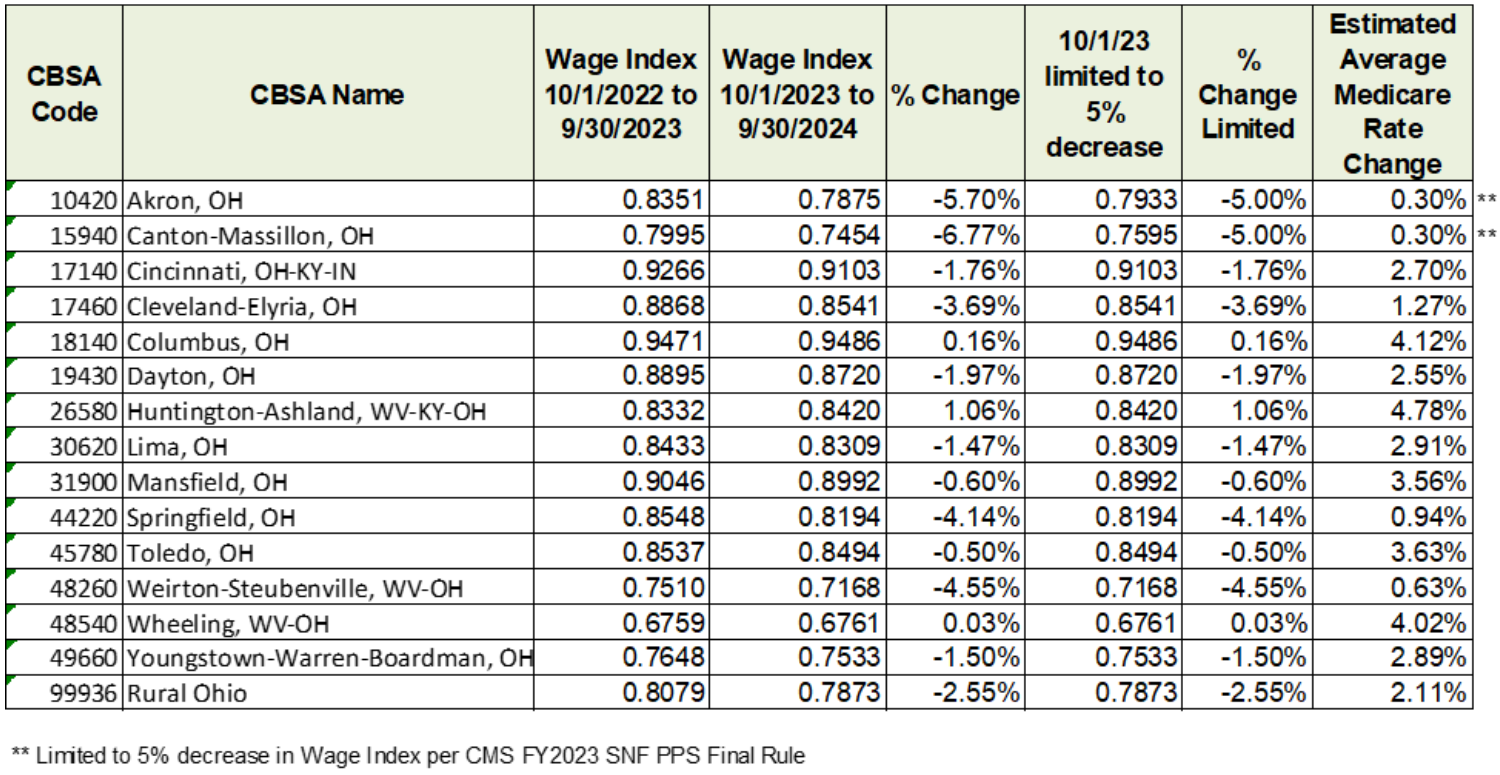
UPDATE: CMS published a correction notice on October 4, 2023 impacting PDPM rates for all CBSAs nationwide. The correction resulted in very minor reductions in most of the wage adjusted PDPM components. We have updated the Ohio CBSA PDPM rates in the links below.
The Centers for Medicare & Medicaid Services (CMS) published the final rule updating Medicare rates for skilled nursing facilities for federal Fiscal Year (FY) 2024 in the August 7, 2023 Federal Register. The rates will be effective from October 1, 2023 through September 30, 2024. Fiscal year 2024 represents the fifth year of the Patient Driven Payment Model (PDPM) payment system for skilled nursing facilities.
Federal Register. The rates will be effective from October 1, 2023 through September 30, 2024. Fiscal year 2024 represents the fifth year of the Patient Driven Payment Model (PDPM) payment system for skilled nursing facilities.
Last year, CMS implemented a two-year phase-in of a 4.6% parity adjustment to PDPM rates as a result of the new system not being budget-neutral as anticipated. The parity adjustment applied a 2.3% cut to the FY 2023 update and another 2.3% cut to the FY 2024 update.
The FY 2024 final rule also provides for a 6.3% net market basket increase over FY 2023, and as a result, net Medicare reimbursement is expected to increase by 4.0%, which is estimated to increase nationwide SNF payments by approximately $1.4 billion. Due to annual updates in CBSA wage indices, your county’s change in Medicare rates may be higher or lower than the published 4.0% increase.
The wage indices of many Ohio CBSAs experienced declines, in some cases significant. Despite these declines, our estimates of PPS rate changes as of October 1, 2023, show all counties in Ohio will see at least a small increase in SNF PDPM rates. Your facility’s results may vary from our estimates below based on your PDPM utilization.
The final rule also made adjustments to the technical mapping of certain conditions between ICD-10 diagnoses and PDPM groupings. CMS has posted an updated PDPM ICD-10 mapping file on its website to assist providers with coding crosswalks and classification logic.
PDPM continues to be complex and it is critical to ensure facility staff stay abreast of the clinical and billing requirements. We are available to assist you with any questions or issues. Please contact us if you are in need of assistance.
PDPM Rates Effective October 1, 2023
The links in the list below provide detailed calculations of the PDPM rates for each of the 15 CBSAs in Ohio. The rates provided for the individual CBSAs are shown prior to the Quality Reporting Program and Value-Based Purchasing adjustments.
Please select the CBSA from the list below in which your county resides to open a printable PDF file. If you are not sure which CBSA to choose, please click the first link to open a crosswalk between the county names and the CBSA names.
DETAILED CALCULATIONS BY OHIO CBSA NAME
- Akron
- Canton-Massillon
- Cincinnati
- Cleveland-Elyria
- Columbus
- Dayton-Kettering
- Huntington-Ashland (Lawrence County, OH)
- Lima
- Mansfield
- Rural Ohio
- Springfield
- Toledo
- Weirton-Steubenville (Jefferson County, OH)
- Wheeling, WV (Belmont County, OH)
- Youngstown-Warren-Boardman
We have developed a calculator to assist in calculating rates for all PDPM groups. The calculator can assist you in seeing changes in reimbursement over the course of a Part A stay due to the potential impacts of tapering and AIDS diagnoses. Please contact us for more information if you are interested.
These rates are subject to change. If a Correction Notice is issued that affects any Ohio counties, we will update our website links with the new rates.
SNF Value-Based Purchasing Program
Prior to the COVID-19 Public Health Emergency, providers who scored well on the SNF Value-Based Purchasing (VBP) hospital readmission measures had the opportunity to earn an increase to their PDPM rates, while those who ranked lower could lose up to 2% of their PDPM rates. However, as a result of COVID-19, CMS made the decision to suppress the hospital readmission calculations used for SNF VBP for FY 2022 and FY 2023, with most providers seeing a .8% reduction to their PDPM rates in those years.
With the Public Health Emergency now over, CMS will return to the previous VBP calculation and each provider will have its own VBP multiplier depending on performance on CMS’ hospital readmission measure. The baseline period for FY 2024 will be FY 2019 and the performance period will be FY 2022.
The FY 2024 final rule several additional changes to the VBP program. It is unknown at this time how the payment calculations will be changed based on the following:
- FY 2026
- Adoption of Nursing Home Staff Turnover measure
- FY 2027
- Adoption of Discharge Function Score measure
- Adoption of Long Stay Hospitalization per 1,000 Resident Days measure
- Adoption of Percent of Residents Experiencing One or More Falls with Major Injury (Long Stay) measure
- FY 2028
- Replacement of the Skilled Nursing Facility 30-Day All-Cause Readmission Measure (SNFRM) with the Skilled Nursing Facility Within Stay Potentially Preventable Readmissions (SNF WS PPR) measure
CMS is also making the following changes to the payment calculations effective FY 2027:
- Adoption of a Health Equity Adjustment which will provide bonus points in the calculation to SNFs that perform well and whose resident population during the applicable performance period includes at least 20% of residents with dual eligibility status
- Increase of the payback percentage policy under the VBP program from the current 60% to a level such that the bonuses provided to the high-performing, high duals SNFs do not come at the expense of the other SNFs. The estimated payback percentage for the FY 2027 program year is 66%
SNF Quality Reporting Program (QRP)
The SNF PPS Final Rule included several changes to the SNF Quality Reporting Program. The QRP requires SNFs to meet a minimum threshold of satisfactory MDS reporting and quality measures data. Facilities who fail to do so are penalized 2% of their PDPM rates. Facilities are not penalized for performance on the measures.
Changes implemented in the FY 2024 final rule include:
- Adoption of New Measures:
- Discharge Function Score – Effective FY 2025, the measure will assess the percentage of SNF residents who meet or exceed an expected discharge function score and use mobility and self-care items already collected on the Minimum Data Set (MDS)
- Percent of Residents Who are Up to Date on COVID-19 Vaccine – Effective FY 2026, the measure will assess the percentage of residents who meet the Center for Disease Control’s (CDC) most recent guidance regarding COVID-19 vaccines
- Modification of Existing Measure:
- COVID-19 Vaccination Coverage Among Healthcare Personnel (HCP) – Effective FY 2025, the measure will assess the percentage of HCP who meet the CDC’s most recent guidance regarding COVID-19 vaccines. The measure currently assesses the percentage of HCP’s who received the primary vaccination series for COVID-19
- Removal of Existing Measures (Effective FY 2025):
- Application of Percent of Long-Term Care Hospital (LTCH) Patients with an Admission and Discharge Functional Assessment and a Care Plan That Addresses Function
- Application of the IRF Functional Outcome Measures: Change in Self-Care Score for Medical Rehabilitation Patients
- Application of the IRF Functional Outcome Measures: Change in Mobility Score for Medical Rehabilitation Patients
Please see the FY 2024 SNF PPS Final Rule for additional information on each of these measures.
CMS is increasing the SNF QRP Data Completion thresholds for the Minimum Data Set (MDS) Data Items beginning with the FY 2026 SNF QRP. SNFs must report 100% of the required quality measure data and standardized resident assessment data collected using the MDS on at least 90% of the assessments they submit to CMS. Any SNF that does not meet the requirement will be subject to a reduction of two percentage points to the applicable FY annual payment update beginning with FY 2026.
HW Healthcare Advisors
Our team consists not only of CPAs, but also highly trained and experienced billing/revenue cycle consultants, certified medical office managers and LNHAs. We are dedicated to working with the regulatory, operational and reimbursement challenges that providers face in an ever-changing healthcare environment.
We can assist you in streamlining your processes, optimizing your operations and identifying potential opportunities and risks. Please contact any of our HW Healthcare Advisors to discuss how we can help you and your facility stay on the path to success.
@2023

Principal
steven.anderson@hwco.cpa