The Ohio Department of Medicaid (ODM) has finalized the fiscal year (FY) 2023 Medicaid rates for Ohio nursing facilities (NF) effective 7/1/2022 to 12/31/2022 using the provisions in the biennium budget bill, HB 110, including additional funding for the quality incentive payments and a correction to the ancillary/support price. The statewide average 7/1/2022 Medicaid rate was $231.72, which was an increase of $10.11 (4.6%) from the 1/1/2022 statewide average rate of $221.62. Peer group 1-L had the largest rate increase at 5.7%, while peer group 3-S had the smallest increase at 3.6%.
The Ohio Department of Medicaid (ODM) has finalized the fiscal year (FY) 2023 Medicaid rates for Ohio nursing facilities (NF) effective 7/1/2022 to 12/31/2022 using the provisions in the biennium budget bill, HB 110, including additional funding for the quality incentive payments and a correction to the ancillary/support price. The statewide average 7/1/2022 Medicaid rate was $231.72, which was an increase of $10.11 (4.6%) from the 1/1/2022 statewide average rate of $221.62. Peer group 1-L had the largest rate increase at 5.7%, while peer group 3-S had the smallest increase at 3.6%.
Rate changes were primarily comprised of the following:
- Semi-annual case-mix adjustment using the average of the 12/31/2021 and 3/31/2022 case mix scores.
- Recalculation of quality incentives including an additional $100 million of funding. The price per point was $1.82, up from $1.32. Facilities are excluded from quality if they are below the 25th percentile of 10.75 points or a Special Focus Facility.
- ODM determined that they overestimated the number of Medicaid days for the Fiscal Year 2022 when they rebased the ancillary/support cost center on 7/1/2021. The correction results in an increase to the ancillary/support price at 7/1/2022 of $.43 – $.88 depending on the peer group.
- Peer Group Price change as a result of moving between Large (100+ beds) and Small (<=99beds) peer groups or Critical Access Add-On change.
Medicaid rates will be recalculated on 1/1/2023 for the semi-annual case-mix adjustment using the average of the 6/30/2022 and 9/30/2022 case mix scores. The quality incentive payment will not change until 7/1/2023.
There was a recent proposal to rebase direct care rates in part to offset the increasing costs of labor and agency usage. We estimate the rate increase would have been in the $25 per day range. The proposal did not pass before the legislature went on summer break. We will keep you posted on any new developments.
As always, the updated rates will impact payments for both traditional Medicaid and MyCare Ohio Medicaid residents. Be sure to review your MyCare payments carefully as the MyCare plans have had issues in the past.
Review your rate package for accuracy
Rate packages are currently available in MITS. Rate reconsideration requests must be filed within 30 days after the later of the date of the rate-setting package notification or the effective date of the rate. It is important that you review these calculations closely for possible errors and submit a timely request for reconsideration. Contact us if you need assistance.
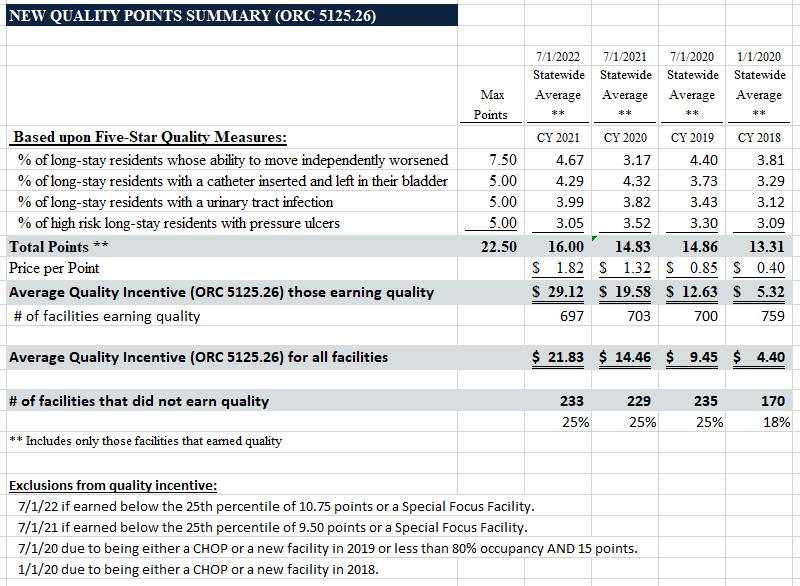
Quality Incentive Summary (ORC 5125.26)
The average quality incentive increased to $21.83 from $14.46. This was primarily due to increased value per quality point of $1.82, up from $1.32, resulting from the additional funding provided by HB 110 in FY2023. The average points earned increased to 16.00 from 14.83. There were 233 providers (25%) that did not receive a quality payment due to the provision excluding facilities that earned below the 25th percentile of 10.75 points and those included on CMS’s Special Focus Facility list. The quality incentive payment is effective for all of FY2023.
The following chart provides more details on average points and the number of facilities earning points:
Please contact us for assistance with any of the following:
- Reviewing your July 1, 2022 Medicaid rate
- Filing a rate reconsideration
- Detailed Ohio Medicaid rate history, case-mix, and quality analysis
- Benchmarking expenses, census and staffing against selected competitors, as well as county, peer group and statewide averages – 2021 Benchmarking Reports will be available soon!
- Medicaid and Medicare cost reporting and rate analysis
- Certificate of Need Projections
- Monthly billing services
- Accounts receivable aging review
- Assistance with Provider Relief Fund reporting
- PRF Compliance Audits and other program-specific government audits
- Any other reimbursement, revenue cycle, accounting, or tax needs

Principal
paula.reape@hwco.cpa